Levodopa is the standard medication used by people with Parkinson's disease. It is usually taken with what is called a peripheral dopa decarboxylase inhibitor - such as benserazide or carbidopa - which will inhibit an enzyme called DOPA decarboxylase (AADC) and prevent levodopa from being converted to dopamine by the body before it reaches the brain. You may know these treatments as Prolopa® (levodopa + benserazide) or Sinemet® (levodopa + carbidopa). They typically limit the side effects caused by high levels of dopamine in the blood and reinforce the action of levodopa in the brain.
However, as time goes by and the disease progresses, many patients experience fluctuations and it becomes necessary to adjust the doses of levodopa: in advanced stages, some patients need doses up to ten times higher than initially given. In recent decades, the question of why levodopa loses its effectiveness has been much debated. While it has long been accepted that this could be related to increased degeneration of dopamine neurons in the brain, recent work has proposed other explanations. Peripheral mechanisms - which do not occur in the brain but in the blood or gastrointestinal tract - could alter the availability of levodopa in the body and thus its effectiveness.
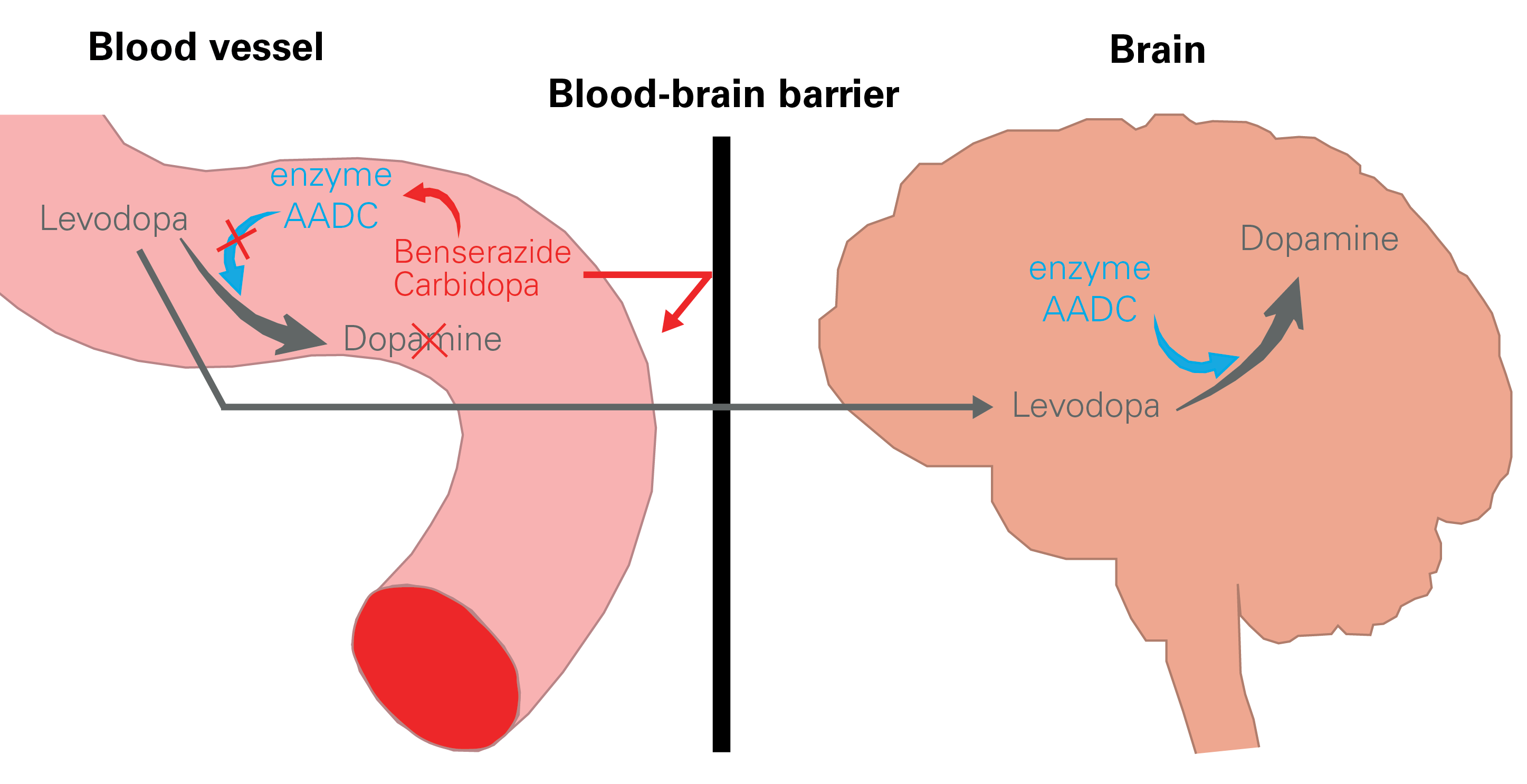
In an article published last March in the scientific journal npj Parkinson's Disease, Dr. Lukas Pavelka and Prof. Rejko Krüger focused on one of these mechanisms in order to better understand why such fluctuations occur in some patients. They studied the effect of chronic use of levodopa in combination with benserazide or carbidopa on the activity of AADC, the enzyme that converts levodopa to dopamine (see diagram above).
They assessed the activity of this enzyme in three independent patient groups, including participants in the Luxembourg Parkinson's Disease Study. They found that the activity of the enzyme is higher in patients using levodopa with benserazide or carbidopa compared to patients not taking this treatment. While it is difficult to understand why these two components would lead to an increase in AADC enzyme activity, the results are interesting: The scientists show that alterations in the activity of this enzyme - which have an impact on the amount of levodopa reaching the brain - could contribute to the reduced efficacy of treatment and the fluctuations observed in patients. This opens the door to new therapeutic strategies that would aim to limit the conversion of levodopa to dopamine in the blood.
Research is underway - continuing blood tests and studies on the role of vitamins and intestinal bacteria in the breakdown of levodopa - to eventually optimize the treatment for each patient.




